Treat 3.2 delivers eligibility and formulary checking, and a new medication history experience
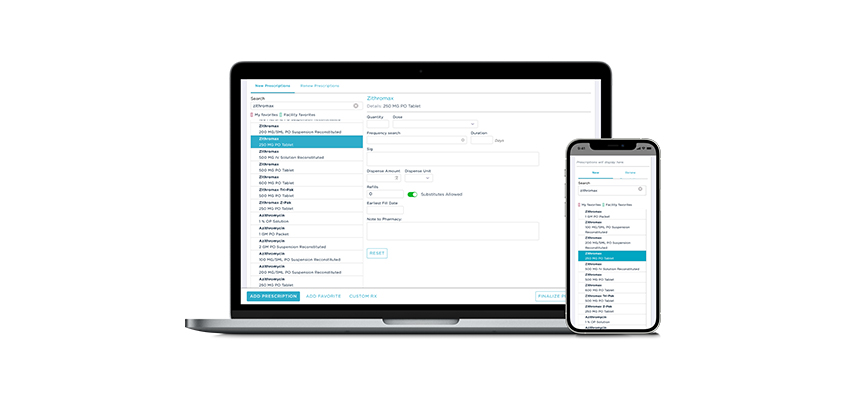
Treat 3.2 brings exciting new features to Treat, including the ability to check eligibility and group level formulary coverage, a more robust medication history experience, and more. Treat 3.2 builds on an improved e-prescribing experience introduced in Treat 3, and will be released today as a free software update.
Eligibility and formulary coverage
Starting today, providers can use Treat to check eligibility and real-time group level formulary coverage, eliminating the need to contact the PBM to verify benefits. These insights can also be used for more-informed conversations with patients.

New medication history interface
Treat 3.2 uses prescription history data and medication information from nearly all major pharmacies and PBMs, enabling clinicians to track all medications patients are taking, even cash pay, to pinpoint patients who may be at risk.

Additional Treat 3.2 features
- Patient Cards get redesigned to make it easier to find the information you use most often.
- PBM support allows you to send the active PBM with an e-prescription for coordination of benefits.